What is Pediatric Obstructive Sleep Apnea and Why is it Important to Diagnose?
Pediatric obstructive sleep apnea (OSA) is a breathing disorder where a child’s airway becomes partially or completely blocked during sleep, causing breathing pauses and disrupted rest. This condition affects approximately 1-5% of children, making it a significant health concern for families in O’Connor and beyond.
The condition manifests through several telltale signs that parents often notice first. Children with OSA typically experience:
- Loud, persistent snoring that occurs most nights
- Restless sleep with frequent tossing and turning
- Breathing pauses or gasping during sleep
- Mouth breathing throughout the night
- Difficulty waking in the morning despite adequate sleep time
- Daytime sleepiness or behavioural problems
These symptoms of OSA in children can easily be dismissed as normal childhood sleep patterns, yet they signal a potentially serious underlying issue requiring medical attention.
The Hidden Dangers of Untreated Sleep Apnea
Untreated pediatric obstructive sleep apnea creates a cascade of health problems that extend far beyond poor sleep quality. Children with undiagnosed OSA face increased risks of:
- Cardiovascular complications including high blood pressure and strain on the heart. The repeated oxygen drops during sleep force the cardiovascular system to work harder, potentially causing long-term damage.
- Cognitive and behavioural challenges such as difficulty concentrating, poor academic performance, hyperactivity, and mood disturbances. Sleep fragmentation prevents the brain from completing essential restorative processes.
- Growth and metabolic issues including failure to thrive and increased obesity risk. Deep sleep stages crucial for growth hormone release become disrupted.
- Dental and facial development problems as chronic mouth breathing can alter jaw structure and tooth alignment.
Early diagnosis through sleep testing O’Connor clinics provides parents with valuable insight into their child’s sleep health, enabling timely intervention to prevent these complications and improve overall wellbeing.
Why Timely Diagnosis Matters
The importance of diagnosis cannot be overstated when considering these far-reaching consequences. Early detection allows for prompt intervention—often through adenotonsillectomy or other treatments—that can reverse many complications before they become permanent.
Accurate diagnosis distinguishes OSA from other sleep disorders and determines severity, guiding appropriate treatment decisions.
How are Sleep Tests Traditionally Conducted for Children?
Traditional pediatric sleep testing relies on in-lab polysomnography (PSG), which remains the gold standard for diagnosing sleep disorders in children. This comprehensive overnight study requires the child to spend a night in a specialised sleep laboratory whilst trained technicians monitor their sleep patterns and physiological functions.
What Does In-Lab Sleep Testing Involve?
Polysomnography involves attaching multiple sensors to the child’s body to capture detailed data throughout the night. The monitoring equipment tracks:
- Brain wave activity through electroencephalogram (EEG) electrodes
- Eye movements via electrooculography (EOG) sensors
- Muscle tone measured by electromyography (EMG)
- Heart rate and rhythm through electrocardiogram (ECG)
- Blood oxygen levels using pulse oximetry
- Breathing patterns via nasal and oral airflow sensors
- Chest and abdominal movement with respiratory effort belts
- Body position and leg movements
A sleep technician remains present throughout the night to observe the child, adjust sensors if needed, and ensure quality data collection. The comprehensive nature of this monitoring allows clinicians to accurately identify sleep-disordered breathing, including obstructive sleep apnoea, and distinguish it from other sleep conditions.
What Challenges Do Families Face with Laboratory Testing?
In-lab sleep tests present several practical obstacles for families in O’Connor and similar communities. The financial burden can be substantial, with full polysomnography costing significantly more than alternative testing methods. Many families face lengthy waiting lists for sleep laboratory appointments, delaying diagnosis and treatment.
The unfamiliar environment poses particular challenges for paediatric patients. Children often struggle to fall asleep in a strange room surrounded by monitoring equipment and wires. Younger children may experience anxiety or fear about sleeping away from home, whilst the presence of sensors can cause discomfort or distress. Some children repeatedly remove sensors during the night, compromising data quality.
Resource demands extend beyond financial costs. Parents must take time off work to accompany their child to the sleep laboratory. Families living in regional areas like O’Connor may need to travel considerable distances to access specialised sleep centres. The sleep laboratory itself requires dedicated space, expensive equipment, and trained overnight staff
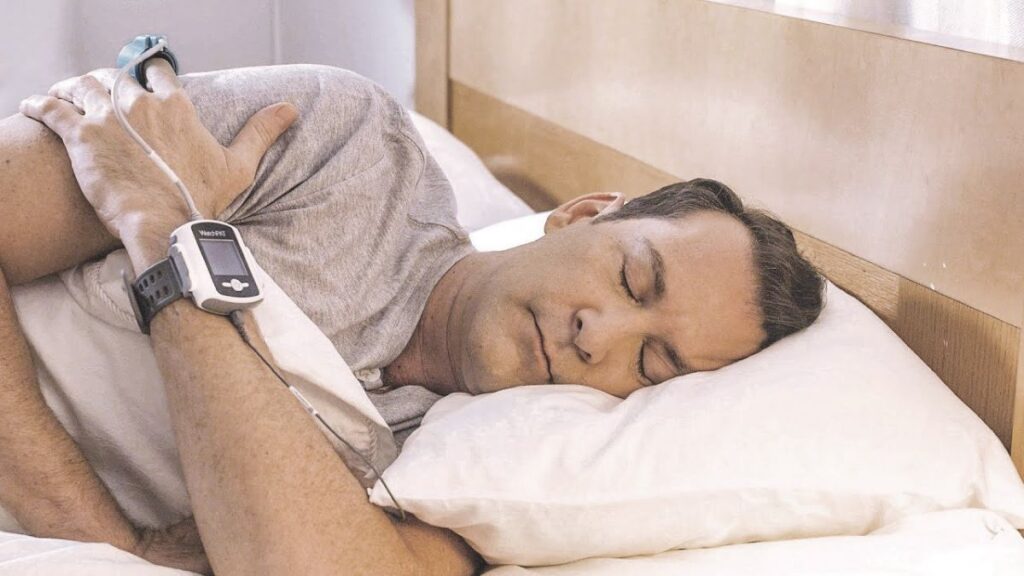
Can Children Take Home Sleep Tests for Diagnosing OSA?
Yes, children can take home sleep tests to diagnose obstructive sleep apnea, and research increasingly supports their use as a practical alternative to laboratory testing. Studies demonstrate that home-based sleep studies for children are both feasible and clinically valuable, particularly for school-aged patients.
The feasibility of home sleep tests for children has been validated through multiple clinical trials examining different age groups and testing methods. Research involving children aged 3-18 years shows that families can successfully conduct sleep studies at home with proper instruction. The familiar environment often yields more representative sleep patterns compared to the artificial laboratory setting, where children may experience anxiety or difficulty falling asleep.
Research Supporting Pediatric Home Testing
Recent studies have examined two primary approaches:
- Type III studies monitoring respiratory parameters through simplified sensor arrays
- Type II polysomnography providing comprehensive data collection similar to laboratory tests
Both methods have demonstrated diagnostic accuracy when applied to appropriate pediatric populations. Children aged 5 years and older show particularly high success rates with home sleep testing, whilst younger children may require additional support or alternative approaches.
Acceptance Among Families and Clinicians
The acceptance of home sleep tests for children extends beyond technical feasibility. Parents appreciate the convenience of testing in their child’s own bedroom, eliminating the stress of overnight hospital visits. The familiar surroundings typically result in more natural sleep behaviour, potentially capturing sleep patterns that better reflect the child’s typical night.
Clinical acceptance has grown as evidence accumulates showing strong correlation between home test results and traditional laboratory findings. The cost-effectiveness of home testing—approximately 63% of full laboratory polysomnography costs—makes diagnosis more accessible to families whilst reducing strain on healthcare resources. Age-appropriate protocols and thorough caregiver training significantly improve test completion rates and data quality.
What Are the Different Types of Home Sleep Tests Available for Children?
There are two main types of home sleep tests available for children, each with different levels of monitoring complexity. The type III sleep study focuses on monitoring breathing, while type II polysomnography at home provides comprehensive data similar to laboratory testing.
Type III Unsupervised Sleep Studies
Type III studies monitor essential respiratory parameters through portable devices that families can operate independently. These tests typically include:
- Pulse oximetry to measure blood oxygen levels
- Nasal cannula to detect airflow patterns
- Thoracoabdominal belts to track breathing effort
Children aged 3-11 years with suspected obstructive sleep apnea can undergo this testing at home without technician supervision. The equipment focuses specifically on identifying breathing disruptions during sleep rather than capturing full brain activity or sleep stages. This streamlined approach makes the test more affordable—approximately 63% the cost of full laboratory polysomnography—whilst still reliably detecting severe OSA cases.
Type II Polysomnography Conducted at Home
Type II polysomnography represents a more comprehensive option for home-based pediatric sleep tests. This method includes nearly all the monitoring channels used in laboratory studies:
- Brain wave activity (EEG)
- Eye movements
- Muscle tone
- Heart rhythm
- Respiratory measurements
- Oxygen saturation
The primary difference from laboratory testing lies in the setting rather than the scope of data collection. Children aged 5-18 years typically receive this testing when clinicians require detailed sleep architecture information alongside respiratory measurements. The familiar home environment often produces more representative sleep patterns, with studies showing increased REM sleep and better sleep efficiency compared to laboratory recordings. This testing option reduces waiting times for diagnosis whilst maintaining diagnostic accuracy comparable to traditional in-lab studies.
How Effective and Reliable Are Home Sleep Tests in Children?
Can home sleep tests accurately diagnose sleep apnea in children? Yes, research demonstrates that home sleep tests can effectively identify obstructive sleep apnea in pediatric patients, though the accuracy of home sleep tests varies by test type and patient age.
Reliability of Type III Unsurpervised Sleep Studies
Type III unsupervised sleep studies show strong reliability in pediatric patients when detecting severe OSA. These tests successfully identify children with significant breathing disturbances during sleep, making them valuable screening tools for adenotonsillar hypertrophy cases. The challenge lies in their failure rates, which reach approximately 29% across studies. Younger children experience higher failure rates than their school-aged counterparts, primarily due to sensor displacement during sleep. Preschool children may move more frequently, dislodging oximetry probes or nasal cannulas that capture critical respiratory data.
Diagnostic Agreement of Type II Home Polysomnography
What about Type II home polysomnography? The diagnostic agreement with lab PSG reaches impressive levels of 87-94%, establishing home T2PSG as a highly reliable alternative for children aged 5-18 years. This comprehensive monitoring captures sleep architecture and respiratory events with precision comparable to laboratory studies.
Differences Between Home and Lab Testing
Home T2PSG often reveals more representative sleep patterns than lab testing. Children sleep in familiar surroundings, resulting in:
- Increased REM sleep duration
- Higher sleep efficiency percentages
- More natural sleep behaviours
- Reduced anxiety-related sleep disruptions
The discrepancies between home and lab results typically involve mild OSA cases rather than moderate or severe presentations. This pattern suggests home testing performs exceptionally well for children requiring immediate intervention whilst potentially missing borderline cases that might benefit from follow-up evaluation.
Cost-effectiveness of Home Sleep Tests
Cost-effectiveness remains significant even accounting for test failures. Type III studies cost approximately 63% of full polysomnography, making repeated testing financially viable when initial attempts fail. Proper caregiver training on sensor placement substantially reduces failure rates, improving the reliability in pediatric patients across age groups.
What Challenges Exist When Using Home Sleep Testing in Children?
Sensor loss creates the primary obstacle, with approximately 29% of home sleep tests failing to produce usable data. Oximetry sensors prove particularly problematic, frequently becoming dislodged during the night when children move, roll over, or unconsciously remove the equipment. This represents one of the most significant challenges in paediatric home sleep testing.
The age factor dramatically influences success rates. Preschool-aged children present considerably more difficulties compared to their school-aged counterparts. Younger children naturally move more during sleep, have smaller fingers that make sensor attachment challenging, and lack the understanding to keep equipment in place throughout the night. These data quality concerns mean families may need to repeat tests, extending the diagnostic timeline.
Common Sensor Adherence Issues Include:
- Oximetry probe displacement – the most frequent cause of test failure
- Nasal cannula dislodgement – particularly when children sleep face-down or move frequently
- Thoracoabdominal belt shifting – though this sensor demonstrates better reliability than others
- Complete equipment removal – more common in very young or anxious children
The challenges in paediatric home sleep testing extend beyond simple equipment issues. Children who are anxious about wearing unfamiliar devices may resist the setup process entirely. Some experience heightened awareness of the sensors, leading to disrupted sleep patterns that fail to represent their typical rest. Parents report frustration when tests fail after careful preparation and a full night of monitoring.
Wireless sensor technology continues to evolve, yet current devices still require multiple attachment points on small, active bodies. The balance between comprehensive data collection and practical wearability remains difficult to achieve, especially for children under five years old who represent the demographic most likely to have adenotonsillar hypertrophy requiring assessment. Click here to get how to get tested without an overnight clinic stay.
How Can Families in O’Connor Prepare for Home Sleep Testing for Their Children?
Proper preparation significantly reduces the risk of test failure and ensures accurate results. Families in O’Connor should begin by scheduling a pre-test consultation where healthcare providers demonstrate the equipment and walk through each component of the device setup.
Essential preparation steps include:
- Understanding the equipment: Caregivers need hands-on practice with each sensor, including the oximetry probe, nasal cannula, and thoracoabdominal belts before taking the device home
- Creating a conducive sleep environment: Remove potential distractions and maintain the child’s regular bedtime routine to encourage natural sleep patterns
- Reviewing troubleshooting protocols: Know what to do if a sensor becomes dislodged or the device indicates an error during the night
- Practising sensor placement: Many families benefit from a trial run the night before the actual test to familiarise children with the sensation of wearing the equipment
Caregiver training forms the cornerstone of a successful paediatric sleep study at home. Research demonstrates that proper training in sensor placement directly correlates with lower failure rates, particularly for the oximetry sensor which proves most vulnerable to displacement. Healthcare providers should ensure caregivers can confidently secure each sensor and recognise proper signal indicators.
The thoracoabdominal belt typically requires special attention during training sessions. Caregivers must learn to position it snugly enough to detect breathing movements without causing discomfort that might wake the child. Some centres provide instructional videos or written guides families can reference during the testing night.
Age-specific considerations matter when preparing for home sleep test:
- Younger children may need gradual desensitisation to wearing sensors during daytime play
- School-aged children often respond well to simple explanations about why the test helps them sleep better
- Involving children in the preparation process increases cooperation and reduces anxiety about the unfamiliar equipment
When Should Traditional In-Lab Polysomnography Still Be Considered?
Traditional in-lab polysomnography (PSG) is still the preferred method of diagnosis for children under three years old. This is because it can be difficult to keep sensors on and get cooperation from very young children during home sleep tests. In fact, very young children are more likely to move the sensors around during home testing, which can result in incomplete or unreliable data that may require additional studies.
Indications for lab PSG
There are certain situations where lab PSG is recommended, in addition to age considerations:
- Children with suspected complex pediatric cases involving multiple medical conditions such as neuromuscular disorders, craniofacial abnormalities, or genetic syndromes
- Patients requiring continuous EEG monitoring to differentiate between sleep-disordered breathing and seizure activity
- Cases where initial home sleep testing produced inconclusive or technically inadequate results
- Children with suspected central sleep apnea or periodic limb movement disorder, which require comprehensive brain wave and leg movement monitoring
The limitations of home testing become particularly evident when detailed sleep architecture analysis is essential for diagnosis. Laboratory environments provide controlled conditions with trained technologists who can immediately address sensor displacement, adjust equipment, and ensure complete data capture throughout the night. Children with developmental delays or behavioural challenges often benefit from the structured support available in supervised laboratory settings, where staff can help maintain sensor placement and provide reassurance during the study.

Is Home Sleep Testing a Viable Option for Children in O’Connor?
Yes, pediatric home sleep testing is a viable option for many children in O’Connor, particularly those aged 5 years and older with suspected obstructive sleep apnea. The evidence demonstrates that both Type II and Type III home studies can accurately diagnose OSA when age and cooperation levels are appropriate.
The benefits and limitations create a clear picture for families. Home testing offers significant advantages including reduced costs (approximately 37% savings even with potential retests), shorter waiting times, and the comfort of the child’s familiar bedroom environment. Type II home polysomnography shows diagnostic agreement rates of 87-94% with laboratory studies, whilst Type III studies effectively identify severe cases requiring urgent intervention.
Age remains the primary consideration. School-aged children typically complete home studies successfully, whilst preschoolers face higher failure rates due to sensor displacement. The thoracoabdominal belt sensor demonstrates better reliability than oximetry in younger patients, and proper caregiver training substantially improves outcomes.
Sleep Testing in O’Connor: Can Children Take a Home Sleep Test Too? The answer depends on individualised assessment. A blended approach serves families best—home testing for straightforward cases in cooperative children, laboratory polysomnography for complex presentations or very young patients. Local sleep specialists can guide families toward the most appropriate testing method based on their child’s specific circumstances, ensuring accurate diagnosis whilst maximising convenience and minimising stress for both children and parents.
FAQs about Sleep Testing in O’Connor:
Pediatric obstructive sleep apnea (OSA) is a condition where a child’s airway becomes blocked during sleep, causing breathing pauses and restless nights. Early diagnosis is crucial because untreated OSA can lead to behavioural issues, poor growth, heart problems, and learning difficulties.
2. What Are the Common Symptoms of Sleep Apnea in Children?
Common signs include loud, persistent snoring, restless sleep, mouth breathing, gasping for air, difficulty waking up, and daytime sleepiness. Parents in O’Connor should seek medical advice if these symptoms occur frequently.
3. How Is Pediatric Sleep Apnea Traditionally Diagnosed?
The gold-standard diagnostic test is in-lab polysomnography (PSG). During this overnight study, sensors monitor brain activity, breathing, oxygen levels, heart rhythm, and body movements while the child sleeps in a specialised sleep laboratory.
4. Can Children Take Home Sleep Tests to Diagnose Sleep Apnea?
Yes, many children can undergo home sleep testing with simplified monitoring equipment. Home tests are less intimidating, more affordable, and allow children to sleep in their familiar environment, often leading to more accurate sleep data.
5. What Are the Different Types of Home Sleep Tests for Children?
There are two main types:
Type III Sleep Study: Measures breathing effort, airflow, and oxygen levels.
Type II Polysomnography: Provides detailed data, including brain waves and heart rhythm, similar to a lab test.
Both are effective, with Type II being more comprehensive.
6. How Reliable Are Home Sleep Tests for Diagnosing Sleep Apnea in Children?
Studies show home sleep tests are up to 87–94% accurate compared to in-lab tests for children aged 5 and above. Proper caregiver training and secure sensor placement greatly improve data reliability and reduce test failure rates.
7. What Challenges Do Families Face with Pediatric Home Sleep Testing?
The main challenges include sensor dislodgement, especially in younger children who move frequently during sleep. Preschoolers may also resist wearing sensors. Caregiver training and trial runs before the test help improve success rates.
8. When Is an In-Lab Sleep Study Still Recommended for Children?
Lab-based testing remains essential for:
Children under 3 years old
Complex cases involving neurological or genetic conditions
Suspected central sleep apnea or seizure disorders
Inconclusive home test results
9. Is Home Sleep Testing a Good Option for Families in O’Connor?
Yes. For most school-aged children with suspected OSA, home sleep testing offers a practical, cost-effective, and comfortable solution. However, very young or medically complex children may benefit from supervised in-lab polysomnography for the most accurate diagnosis.




